Introduction
Sialadenitis is defined as inflammation of the salivary gland. It can be acute or chronic, and there is a wide array of potential causes, from infection to autoimmune. It most commonly affects the parotid gland
Aetiology
Causes of sialadenitis can be divided up into:
- Infective (viral or bacterial, as discussed below)
- Stones (60% of cause of sialadenitis)
- Malignancy
- Autoimmune, including Sarcoidosis*, Sjögren’s syndrome, systemic lupus erythematosus or Wegener’s granulomatosis
- Idiopathic
*Heerfordt’s syndrome is a form of sarcoidosis, composed of a triad of parotid enlargement, anterior uveitis, and facial nerve palsy
Viruses are more common than bacteria as pathogens causing sialadenitis. Of viral causes, mumps is the most common, affecting either the parotid (more common) or the submandibular gland, yet other viral causes include coxsackie, parainfluenza, and HIV*.
Common bacterial causes include S. aureus (most common), S. viridans, H. influenzae, and Strep. pyogenes. Apart from recurrent infections secondary to sialolithiasis, chronic sialadenitis is most commonly associated with autoimmune diseases such as Sjögren’s syndrome or sarcoidosis.
*HIV parotitis is classically either a non-painful swelling or asymptomatic
Mumps
Mumps parotitis is caused by the mumps virus, a highly contagious virus transmitted by respiratory droplets or direct contact.
Patients complain of prodromal symptoms lasting a few days, including a low grade pyrexia, headache, and malaise. Patients will then develop bilateral gland swelling (although can be unilateral). Complications of the disease include meningitis / encephalitis, deafness, pancreatitis, and orchitis.
Mumps is a preventable disease with use of the MMR vaccination, however there is no cure and treatment is purely supportive. It is a notifiable disease.
Clinical Features
Patients will commonly report painful swelling and tenderness of the gland (Fig. 2). Pyrexia, lymphadenopathy, and erythema of the affected gland can also develop. The area may be fluctuant to palpate if there were any abscess formation.
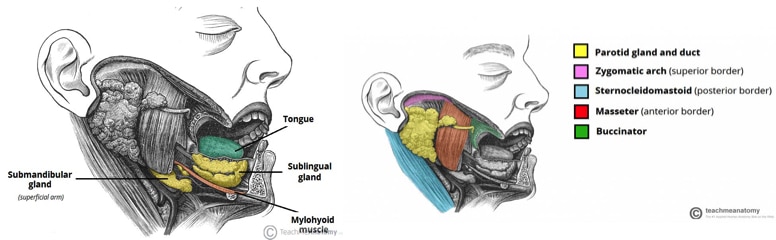
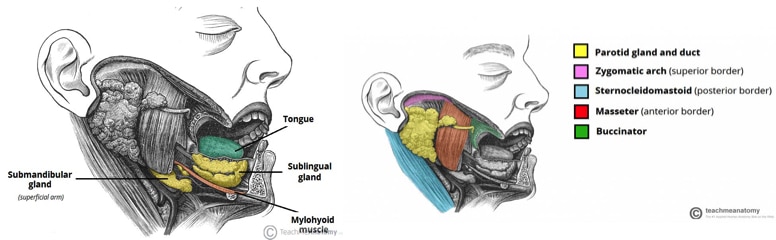
On examination of the oral cavity, bimanual palpation of the salivary glands should be performed, whilst inspecting the oral cavities for the ductal orifices – infectious causes may result in a purulent discharge from the duct, alongside any additional symptoms from any potential abscess formation (e.g. pyrexia, rigors).
Investigations
Routine bloods (FBC, CRP) will identify any infective cause; any suspicion of autoimmune disease, serum ESR, and autoimmune screen bloods will be warranted.
Pus swabs should be taken if possible and blood cultures if any evidence of systemic involvement. If mumps is suspected, suitable viral serology can also be tested.
If there is suspicion of malignant disease, an ultrasound-guided fine needle aspiration cytology should be performed to aid diagnosis.
Imaging
Ultrasound scan will identify any solid masses or fluid collections suspected within the glands, or to identify any ductal calculi which may be causing the infection. A CT scan may be requested if there are any suspicion of deep neck space abscess or malignancy.
Management
Most cases of sialadenitis can be managed conservatively. This involves ensuring adequate oral hydration and analgesia (including NSAIDs and paracetamol), alongside moist heat.
Artificial saliva can be used in cases where saliva production is impaired. Patients can trial sialogogues, such as lemons or sour sweets, to encourage saliva production. Regular massage and milking the glands can also help with the inflammation.
Antibiotics should be given if bacterial sialadenitis is suspected, with choice of empirical antibiotics based upon local guidelines.
Any cases of abscess formation will warrant an incision and drainage. Patients with recurrent sialadenitis may benefit from surgical removal of the gland (depending on the cause), but this is uncommon.
Prognosis
Most cases of acute sialadenitis recover well with conservative and medical management. However, untreated severe cases can develop into deep neck space infection, leading to airway obstruction.
Patients with recurrent infections, secondary to calculi or autoimmune causes, can develop into chronic sialadenitis. This results in hardening of the salivary gland and lower salivary production, in turn increasing risk of tooth decay.
Key Points
- Sialadenitis is inflammation of the salivary glands, most commonly caused from a viral pathogen
- The most common symptom is a painful swelling and tender gland
- Diagnosis is clinical, however imaging can be required if complications are suspected
- Most patients are managed conservatively with hydration and analgesia