Sepsis is the life-threatening organ dysfunction caused by an abnormal and uncontrolled host response to an infection.
It is the leading cause of death in intensive care units, and has an overall mortality of 30-40%. It is a condition that is essential to identify and treat early and aggressively, as any patient admitted to hospital with sepsis has a 10% increased risk of mortality.
In this article, we shall look at the clinical features, investigations and management of sepsis.
Sepsis Criteria
The criteria for sepsis aim to aid the early identification of patients developing (or with) a clinical picture of sepsis. There are two criteria both required for a diagnosis of sepsis:
- Presence of a known or suspected infection
- Clinical features of organ dysfunction
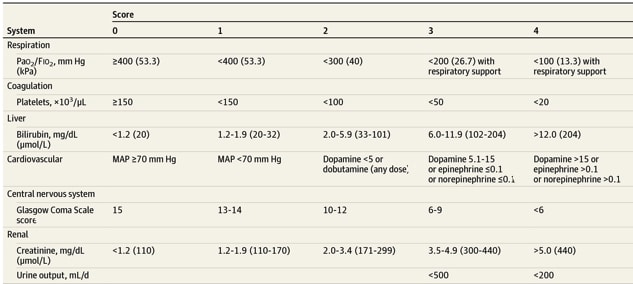
- Calculating a ‘SOFA score’ (Fig. 1) is a means by which clinicians can quantify the level of organ dysfunction
For a patient with a known or suspected infection, a SOFA score greater than or equal to two indicates sepsis; the SOFA score can also be used to monitor and quantify a patient’s clinical course and response to treatment for sepsis.
Note: The previous sepsis criteria was found to be present in many hospital patients who never actually developed infection or incurred any adverse outcomes, alongside 1 in 8 patients admitted to ICU with infection and organ failure not meeting the criteria for sepsis
qSOFA score
The qSOFA score is a shortened version of the full SOFA criteria. It was developed to allow for the rapid assessment of potential sepsis, based purely on clinical signs.
The qSOFA score permits the diagnosis of potential sepsis to be made prior to any investigations and can be completed by any healthcare professional.
Any patient with a known or suspected infection and a qSOFA score ≥2 should be investigated and managed for sepsis as necessary. The qSOFA criteria are:
- Respiratory Rate ≥ 22/min (1 point)
- Altered Mental State (1 point)
- Systolic Blood Pressure ≤100mmHg (1 point)
Investigations and Management
For any patient diagnosed with sepsis, immediate investigation and management steps are vital.
These steps are commonly referred to as the “sepsis six” and should be completed within one hour of diagnosing sepsis:
| 1 | Oxygen | Start 15L O2 via a non-rebreathable mask, aiming for target saturations 94-98% (or 88-92% in chronic retainers), only titrating once appropriately saturating |
| 2 | IV fluid therapy | 500-1000mL initial fluid bolus, followed by ongoing fluid status re-assessment |
| 3 | Blood cultures | Take blood cultures prior to administering antibiotics, along with any other relevant cultures from the suspected infection site |
| 4 | IV antibiotics | Start empirical antibiotics (based on local guidelines), before switching to targeted therapy when sensitivities are available |
| 5 | Routine bloods, inc. lactate | Routine bloods should include FBC, U&E, LFTs, clotting, CRP, and glucose; lactate can be quickly be assessed rapidly from a blood gas |
| 6 | Monitor urine output | Catheterise the patient if appropriate and accurately monitor urine output; aim for at least >0.5mL/kg/hour |
Ensure that your seniors are involved early in the care of these patients. Ask the nursing staff to take hourly observations and to inform you if there is any deterioration of the patient.
Further management may include assessment by intensive care teams and commencing vasopressor agents (e.g. noradrenaline), renal replacement therapy, and/or ventilator support.
Source Identification
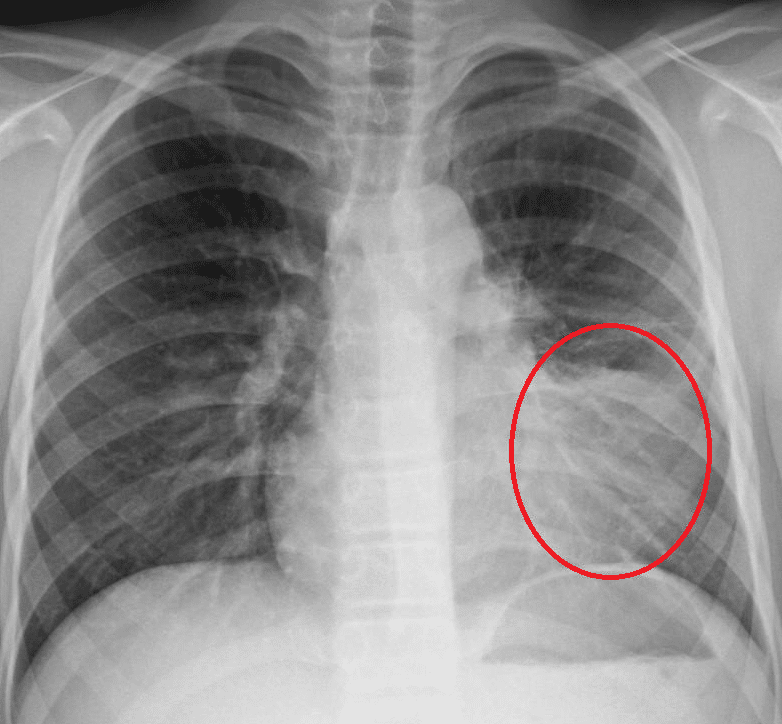
Figure 2 – A CXR showing left lower zone consolidation
Identification of the infection source is important in the investigation of sepsis cases. Appropriate investigations may include:
- Urine dip +/- culture
- Chest X-ray (CXR)
- Swabs (e.g. surgical wounds)
- Operative site assessment (via CT or US imaging)
- Cerebrospinal fluid sample (via LP)
- Stool culture
Escalating Management
Whilst many septic patients can be managed in the ward environment with early senior support, involvement of intensive care / clinical outreach teams should be considered when:
- Evidence of septic shock
- Lactate > 4.0mmol
- Failure to improve from initial management
Sepsis on Surgical Wards
The common sources of pyrexia in a surgical patient can be remembered using the Seven C’s:
- Chest (infection)
- Cut (wound infection)
- Catheter (UTI)
- Collections (abdomen, pelvic etc.)
- Calves (DVT)
- Cannula (infection, if applicable)
- Central line (infection, if applicable)
Septic Shock
Septic shock is defined as sepsis with hypotension, despite adequate fluid resuscitation or requiring the use of inotropic agents to maintain a normal systolic blood pressure.
Management usually involves aggressive fluid resuscitation and antibiotic therapy, with the likely involvement of the critical care team. Inotropes are often used to maintain organ perfusion.
Key Points
- Sepsis is the life-threatening organ dysfunction caused by an abnormal and uncontrolled host response to an infection
- Criteria for the diagnosis of sepsis is the presence of a known or suspected infection with clinical features of organ dysfunction
- Early identification is essential in its management
- The “Sepsis 6” can aid in its initial investigation and management